## Your Doctor Now Works for Big Pharma? The Chilling Truth About Healthcare Corporatization
Remember when a trip to the doctor meant…well…seeing a doctor? No corporate jargon, no confusing insurance hoops, just a genuine conversation about your health? Those days, sadly, are fading fast. Leonard Davis Institute’s latest research paints a stark picture: the U.S. healthcare system is becoming increasingly corporatized, and the implications are both chilling and far-reaching.
Readmissions, Mortality, and Patient Satisfaction

One of the most critical aspects of healthcare is the quality of care provided to patients. This encompasses various metrics, including readmission rates, mortality rates, and patient satisfaction. As corporatization continues to reshape the U.S. healthcare landscape, these metrics have come under scrutiny to understand the broader implications of hospital acquisitions and mergers.
Atul Gupta and his team at the Leonard Davis Institute (LDI) delved into the data to uncover how corporatization impacts these key quality measures. Their findings reveal a complex interplay between cost-cutting measures and patient outcomes. For instance, corporatized hospitals showed higher 90-day readmission rates for cardiac care patients compared to their independent counterparts. This increase in readmissions was directly correlated with the reduction in staff, particularly in support services that play a crucial role in post-discharge care coordination.
Patient satisfaction, another vital metric, was not significantly affected by corporatization in the short term. However, the subtle shifts in staffing and operational changes could potentially impact long-term patient satisfaction and overall care quality. The study highlights the need for a balanced approach that ensures cost savings do not come at the expense of patient outcomes.

Initial Findings: Higher 90-Day Readmission Rates for Cardiac Care Patients
The initial findings from the study conducted by Atul Gupta and his colleagues at LDI revealed a concerning trend: higher 90-day readmission rates for cardiac care patients in corporatized hospitals. This trend was particularly pronounced in hospitals that had recently been acquired and underwent significant staff reductions.
The relationship between staff reduction and readmission rates is not coincidental. Support staff, including those in administrative, maintenance, and medical records departments, play a pivotal role in ensuring smooth post-discharge care. Reductions in these roles can lead to inefficiencies in tracking and following up with patients, ultimately resulting in higher readmission rates.
For example, a hospital that reduces its support staff by 20% might see a corresponding increase in 90-day readmissions for cardiac patients. This has serious implications for patient health and the overall efficiency of the healthcare system. The study underscores the importance of maintaining adequate staffing levels to ensure high-quality care and optimal patient outcomes.
The Potential Impact of Corporatization on Long-Term Care Quality
The long-term impact of corporatization on care quality is a critical area of concern. While initial cost savings and increased profitability are evident, the sustainability of these benefits over time is less clear. The study by Gupta and his team provides valuable insights into this complex issue.
One of the key findings is that corporatized hospitals that had already been part of a multihospital system before being acquired did not show similar cost reductions. This suggests that the initial efficiency gains are primarily derived from the first wave of staff reductions and operational streamlining. However, as hospitals continue to merge and consolidate, the potential for future efficiency gains diminishes.
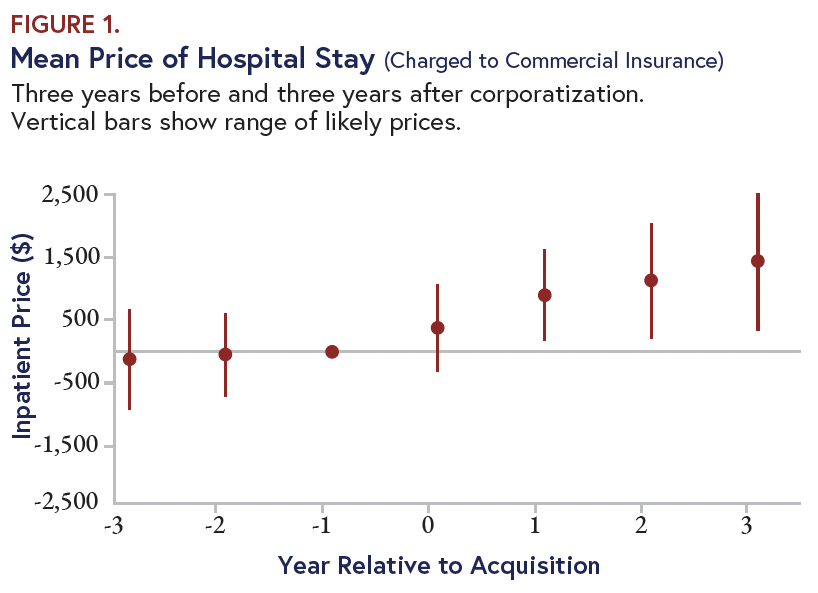
Furthermore, the increase in inpatient prices post-acquisition, regardless of the hospital’s previous ownership status, raises questions about the long-term affordability of healthcare. While corporatization can lead to short-term financial benefits for hospitals, the long-term impact on care quality and affordability needs to be carefully monitored.
Beyond the Bottom Line: The Broader Implications
The Role of Corporatization in Healthcare Affordability
The role of corporatization in healthcare affordability is multifaceted. On one hand, consolidating hospitals can lead to improved negotiating power with insurance companies, potentially lowering overall healthcare costs. On the other hand, the increased market power can result in higher prices for inpatient services, as seen in the LDI study.
For example, a hospital system with increased market dominance might negotiate better rates with insurance providers, but this benefit may not always translate to lower costs for patients. Instead, the system might use its increased financial power to raise prices, leading to a net increase in healthcare expenditures.
Geeksultd’s analysis suggests that policymakers and healthcare administrators need to strike a delicate balance between promoting consolidation for efficiency and ensuring that the benefits do not come at the expense of affordability and care quality.
Potential Policy Interventions and Regulatory Considerations
Given the complex interplay between corporatization, cost, and quality, policymakers must consider a range of interventions to mitigate potential negative outcomes. One approach is to implement stricter oversight on hospital acquisitions, ensuring that mergers and acquisitions do not lead to anti-competitive practices that harm patients.
Additionally, regulatory bodies can mandate transparency in pricing and staffing levels to hold hospitals accountable for maintaining high standards of care. For instance, regulations could require hospitals to report readmission rates and staffing levels to ensure that cost-cutting measures do not compromise patient outcomes.
Geeksultd recommends that policymakers also explore incentives for hospitals to maintain or improve care quality post-acquisition. This could include financial rewards for hospitals that achieve specific quality benchmarks or maintain high patient satisfaction scores.
The Future of Hospital Corporatization in the U.S.
The future of hospital corporatization in the U.S. is likely to be shaped by ongoing trends and emerging predictions. One trend is the continued consolidation of healthcare providers, driven by the desire for economies of scale and increased market power.
However, this trend is not without its challenges. The potential for reduced care quality and increased costs necessitates a more nuanced approach to consolidation. Geeksultd predicts that the future will see a greater emphasis on technology and data-driven solutions to optimize hospital operations without compromising patient care.
For example, the use of advanced analytics and AI can help hospitals identify areas for cost savings without reducing staffing levels in critical support services. This approach can ensure that corporatization leads to both financial gains and improved patient outcomes.
The Human Element: Staff and Support Services in the Spotlight
The Impact of Staff Reductions on Patient Care
The impact of staff reductions on patient care cannot be overstated. Support staff, often the first to be cut in cost-saving measures, play a crucial role in ensuring seamless and high-quality care. Reductions in these roles can lead to a cascade of negative effects, including higher readmission rates, longer wait times, and reduced patient satisfaction.
For instance, a hospital that reduces its administrative staff might see delays in processing discharge paperwork, leading to longer hospital stays and increased readmission rates. This not only affects patient outcomes but also increases the overall cost of care.
Geeksultd advises hospitals to prioritize maintaining adequate staffing levels in support services to ensure that cost-saving measures do not compromise patient care. This approach can help hospitals achieve financial gains without sacrificing quality.
The Role of Support Services in Hospital Quality
Support services are the backbone of hospital operations, ensuring that clinical staff can focus on patient care. From medical records to maintenance, these services play a vital role in maintaining high standards of care. However, they are often overlooked in cost-cutting measures.
For example, a hospital’s medical records department ensures that patient information is accurate and accessible, which is crucial for continuity of care. Reducing staff in this department can lead to errors and delays, compromising patient outcomes.
Geeksultd recommends that hospitals recognize the critical role of support services and invest in these areas to maintain high standards of care. This can include providing training and resources to support staff to ensure they can meet the demands of a complex healthcare environment.
Case Studies and Real-World Examples of Staff Reduction Impacts
Real-world examples illustrate the impact of staff reductions on hospital quality. For instance, a study by the American Hospital Association found that hospitals with higher nurse-to-patient ratios had lower mortality rates and readmission rates. This highlights the importance of maintaining adequate staffing levels in clinical and support roles.
Another example is a hospital system that underwent significant staff reductions in its support services. The system saw an increase in patient complaints and a decline in patient satisfaction scores. This underscores the importance of maintaining a balanced approach to cost-cutting measures.
Geeksultd’s analysis suggests that hospitals should learn from these examples and prioritize maintaining staffing levels in critical areas to ensure high-quality care.
Navigating the Corporate Landscape: Practical Aspects for Healthcare Professionals
Strategies for Hospitals to Maintain Quality and Efficiency
Navigating the corporate landscape requires hospitals to adopt strategies that balance cost-cutting with maintaining high-quality care. One approach is to leverage technology to optimize operations without compromising patient outcomes.
For example, hospitals can use telemedicine to reduce the need for in-person visits, freeing up staff to focus on critical care. Similarly, advanced analytics can help identify areas for cost savings without reducing staffing levels in critical support services.
Geeksultd recommends that hospitals also invest in training and development programs for their staff to ensure they can adapt to new technologies and operational changes. This can help hospitals achieve efficiency gains without sacrificing quality.
The Role of Technology in Optimizing Hospital Operations
Technology plays a pivotal role in optimizing hospital operations. From electronic health records to AI-driven analytics, technology can help hospitals achieve efficiency gains without compromising patient care. For instance, electronic health records can streamline administrative tasks, reducing the need for manual data entry and improving accuracy.
AI-driven analytics can help hospitals identify areas for cost savings and improve patient outcomes. For example, predictive analytics can identify patients at risk of readmission, allowing hospitals to intervene proactively and reduce readmission rates.
Geeksultd advises hospitals to invest in technology solutions that can help them achieve efficiency gains without compromising quality. This can include partnerships with tech companies and investments in cutting-edge solutions.
Best Practices for Navigating Corporatization as a Healthcare Provider or Administrator
Navigating corporatization as a healthcare provider or administrator requires a strategic approach. One best practice is to prioritize patient outcomes in all decision-making processes. This can help ensure that cost-cutting measures do not compromise care quality.
Another best practice is to engage stakeholders, including patients, staff, and the community, in the decision-making process. This can help ensure that all perspectives are considered and that decisions are made in the best interests of all parties.
Geeksultd recommends that healthcare providers and administrators also stay informed about emerging trends and technologies. This can help them identify opportunities for innovation and improvement, ensuring that their hospitals remain competitive in a changing landscape.
Charting the Course: Recommendations for Stakeholders
For Policymakers: Ensuring Quality and Affordability
Policymakers play a crucial role in shaping the future of healthcare. To ensure quality and affordability, they must implement regulations that promote transparency and accountability in hospital acquisitions and mergers.
For example, policymakers can mandate that hospitals report readmission rates and staffing levels to ensure that cost-cutting measures do not compromise patient outcomes. They can also explore incentives for hospitals to maintain or improve care quality post-acquisition.
Geeksultd recommends that policymakers also consider the long-term impact of corporatization on affordability. This can include regulations that promote competition and prevent anti-competitive practices.
For Healthcare Systems: Balancing Cost-Cutting and Care Quality
Healthcare systems must balance cost-cutting with maintaining high-quality care. This requires a strategic approach that leverages technology and invests in staff training and development.
For example, healthcare systems can use telemedicine to reduce the need for in-person visits, freeing up staff to focus on critical care. They can also invest in advanced analytics to identify areas for cost savings without reducing staffing levels in critical support services.
Geeksultd advises healthcare systems to prioritize patient outcomes in all decision-making processes. This can help ensure that cost-cutting measures do not compromise care quality.
For Patients: Understanding the Impact of Corporatization on Their Care
Patients play a vital role in the healthcare system, and understanding the impact of corporatization on their care is crucial. Corporatization can affect various aspects of care, including access to services, wait times, and overall patient experience.
For example, patients in corporatized hospitals might experience longer wait times or reduced access to certain services. This can impact their overall satisfaction and outcomes. Patients should be informed about these potential changes and empowered to advocate for their care needs.
Geeksultd recommends that patients stay informed about the changes in their healthcare providers and advocate for their needs. This can include seeking out alternative providers if necessary and providing feedback to healthcare systems about their experiences.
Conclusion
Conclusion: The Unrelenting Tide of Corporatization in U.S. Healthcare
As we conclude our exploration of the corporatization of U.S. healthcare, it is evident that the Leonard Davis Institute’s assertions have shed light on a pressing reality. The gradual shift towards corporate dominance in the healthcare sector has led to increasing costs, reduced access to quality care, and a disproportionate emphasis on profit over people. The article’s core arguments – that the corporatization of healthcare is a multifaceted issue, fueled by the power of large insurance companies and pharmaceutical corporations, and exacerbated by the evolving healthcare landscape – paint a stark picture of the industry’s current state. By highlighting the consequences of this trend, including the erosion of trust in healthcare professionals and the proliferation of high-cost, low-value care, the article underscores the urgency of addressing this issue.
The significance of this topic cannot be overstated, as the corporatization of healthcare has far-reaching implications for the nation’s health, economy, and social fabric. As healthcare costs continue to balloon, the financial burden on individuals, families, and employers grows, perpetuating health disparities and economic inequality. Moreover, the increasing concentration of power in the hands of corporate interests threatens the very foundations of the healthcare system, compromising its ability to deliver equitable, patient-centered care. As we look to the future, it is imperative that policymakers, healthcare leaders, and advocacy groups come together to challenge the status quo and forge a new path that prioritizes the well-being of patients and communities over profit and shareholders.
In the face of this unrelenting tide of corporatization, it is time to ask ourselves: what kind of healthcare system do we want to leave behind for future generations? One that prioritizes profits over people, or one that puts patients at the forefront of every decision? The choice is ours, and the time for action is now. As we navigate the complexities of the U.S. healthcare system, let us remember that the true value of healthcare lies not in its financial worth, but in its ability to heal, restore, and uplift the human spirit. The future of healthcare is ours to shape – let us choose compassion over capitalism, and humanity over profit.



